Welcome! Below, I have three videos covering the gut-brain axis. The topics that I will cover include:
- A brief history of the central nervous system and the gut-brain axis
- An introduction to the blood-brain barrier (BBB), as well as mechanisms that enable molecules to cross this structure
- An introduction to the gut microbiota and how they can influence host health
Please read the text associated with each video prior to watching it, as it adds context for the video and why it is important to the gut-brain axis.
On Wednesday, during class (later start at 9am), I will be available to answer any questions that you may have about the topics covered, as well as re-explain anything that you found unclear. If time permits, or there are no questions on Wednesday, I will present a case study about how the gut microbiota may be manipulated to treat human disease. While it is not essential, please try to watch the videos prior to class, as it may help your understanding of this case study.
To download a copy of the lecture slides, please click the following link: https://wnzl.ca/PSIA851-GutBrainAxisSlides
Please note: In an attempt to save paper, I have removed slide transitions in the above download. I do not include anything that I scribbled on the slides while recording the videos. The scribbles do not add vital information to the slides, but they may help your understanding.
Note: If the following is unclear upon the first read, I recommend revisiting the following text after watching the videos.
What is the gut-brain axis:
The gut-brain axis is simply defined as any pathway that connects a signal originating in the gut to a response in the brain or vice versa (i.e., the pathway that connects a signal originating in the brain that to a response in the gut). In any gut-brain axis study, it is important to demonstrate the pathway that connects the signal in one organ to the response in the other. It is not adequate to simply measure a parameter in both organs, observe differences in both organs, and then state this is a causative relationship. Let me drive home this point with a fictitious example:
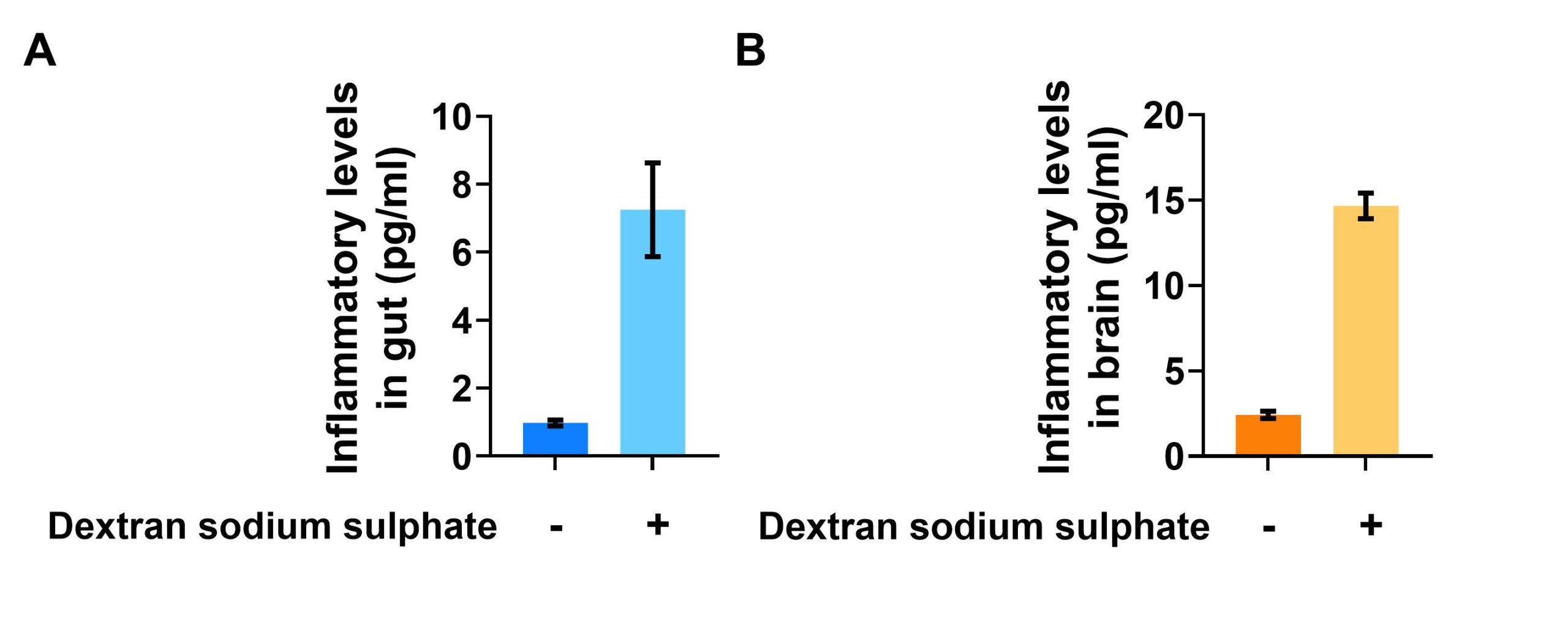
A graph showing levels of inflammatory response in the (A) gut and (B) brain in the presence or absence of a compound called dextran sodium sulphate.
In this example, mice were orally administered (via drinking water) a compound called dextran sodium sulphate. This compound is known to increase inflammatory responses in the gut, as depicted in (A). The researchers, interested in the gut-brain axis, also measured inflammatory responses in the brains of the same mice, as depicted in (B). To their surprise, they observe an increase in inflammatory responses in the brain too! Therefore, these researchers conclude that there exists a gut-brain axis pathway whereby inflammation in the gut causes an increase in brain inflammation.
Not necessarily. There are many pathways that could be responsible for this observation – some could be categorized as a gut-brain axis pathway, while others would not be categorized this way. I will give one example of each:
A possible non-gut-brain axis pathway
Dextran sodium sulphate is a harsh molecule that damages any tissue it is exposed to. Note that dextran sodium sulphate also induces an inflammatory response at any site of tissue damage.
After ingestion, dextran sodium sulphate damages various tissues of the gut epithelia very badly. The gut lining is damaged to such an extent that dextran sodum sulphate is able to leak into the circulatory system. Once in the circulatory system, dextran sodium sulphate gets pumped to the brain vasculature, whereby it is able to directly damage cells of the blood-brain barrier. Once these cells are damaged, dextran sodium sulphate can readily leak into the brain. In the brain, this molecule increases an inflammatory response in the brain.
This example is not an example of a gut-brain axis pathway because the signal causes a change in the brain does not originate from the gut – it originated from the drinking water. In other words, since this relationship is a correlation, it is not a gut-brain axis pathway.
A possible gut-brain axis pathway:
Dextran sodium sulphate is a harsh molecule that damages any tissue it is exposed to. Note that dextran sodium sulphate also induces an inflammatory response at any site of tissue damage.
After ingestion, dextran sodium sulphate damages various tissues of the gut epithelia, but not to the extent that dextran sodium sulphate is able to leak into the circulatory system. Unlike in the above example, this means that dextran sodium sulphate does not enter the circulatory system. So what could happen instead? Well, the inflammatory response in the gut tissue still occurs from the damage. This inflammatory response in the gut causes the gut epithelia to release inflammatory molecules into the circulatory system (as a means to signal to the body that damage has occurred). These inflammatory signals could in turn (1) activate the afferent fibres of the vagus nerve (a pathway termed the inflammatory reflex) which sends an electrical signal to the brain, causing the brain to release inflammatory molecules in the brain, or (2) be pumped to the brain vasculature, subsequently transported across the blood-brain barrier, and then upregulated brain inflammation.
This an example is of a gut-brain axis pathway because the signal causing the change in the brain originated from the gut. That is, the signal that is causing an inflammatory response in the brain were the inflammatory molecules released by the gut. In other words, since this relationship is causative, it is a gut-brain axis pathway.
Why this is information is important:
A gut-brain axis pathway relies on a researcher to be able to explain the pathway that links a gut signal to a brain response (or a brain signal to a gut response). There are now a number of examples in the literature that detail these gut-brain axis pathways. Yet, it is important that the reader critically think about these examples before concluding they are a true gut-brain axis pathway, as several examples in the literature are only correlative relationships and therefore have not been validated as a gut-brain axis pathway.
Examples of gut-brain axis pathways:
- Microbiota-gut-brain axis (some pathways well-described, but the pathways of many are unknown. An example of a well-described pathway is in regards to bile acids).
- HPA-mediated gut-brain axis
- Inflammatory reflex
- Systemic circulation-mediated gut-brain axis
These latter two examples in red will be the focus of this video series. The microbiota-gut-brain axis will be briefly talked about in video 3.
Keep the following at the forefront of your mind as you continue on to the videos:
To be considered a gut-brain axis pathway, there must be a detailed account of how a gut signal causes a change in the brain, or vice versa. Correlative relationships are not a gut-brain axis pathway (but they might be in the future when we understand the pathway better!). In any term paper or exam question regarding the gut-brain axis, I expect that the pathway be detailed enough to demonstrate a causative relationship. A drawing would greatly enhance a readers understanding of the pathway you are describing.
Video 1
In the first video, you will be introduced to this video series, as well as learn the history of the blood-brain barrier (BBB). The gut-brain axis was proposed sixteen years ago, and a majority of the research surrounding this topic was published in the last five years. Thus, our understanding of the gut-brain axis is constantly evolving. To understand why the discovery of the gut-brain axis was monumental, I believe we must (briefly!) appreciate how we got to our present understanding of the central nervous system.
Video 2
In this second video, I will describe the structure of the blood-brain barrier, as well as mechanisms that molecules can engage to cross this structure. This video is entirely about describing possible pathways of the systemic circulation-mediated gut-brain axis. In other words, if a molecule originating in the gut is released into the circulatory system, this video describes 7 possible mechanisms of how that molecules can enter the brain and subsequently alter brain processes.
Video 3
In this third video, I will give an overview of the microbiota-gut-brain axis. Specifically, I will give background information on gut microbes and a brief example about how they can communicate with the brain through the inflammatory reflex or system circulation. In addition, I will describe a few consequences of an abnormal or absent gut microbiota. I will also briefly touch on the limitations of animal models used to study the effects of gut microbiota, and how limitations of these models complicate their translation to the human context.
Note: On a term paper or exam, I would not consider the example I gave on slide 43 about body fat composition a gut-brain axis pathway, as there was no details on how the brain is involved in this example. There are several primary research articles that implicate the brains involvement in this pathway. If these details were added, this would be an acceptable example.
There is no video.
During class, if there is extra time, I will take a much more technical dive into how the gut microbiota can be manipulated to treat human disease, using real data. The specifics of the experiments are complicated (i.e., there will be a lot of vocabulary words), but do not worry about the details. When watching this video, feel free to grab some popcorn (or coffee, tea, etc., if 9am popcorn isn’t your thing) and relax – I simply want to demonstrate the potential importance of the gut-brain axis in therapeutics.